Blogger: Marte Singsås Dragset
Researcher at Centre of Molecular Inflammation Research (SFF-CEMIR), Department of Cancer Research and Molecular Medicine (IKM)
24 March is the World Tuberculosis Day. Here in Norway, most people know tuberculosis (TB) from media, school and vaccination programs. Some people have a parent, grandparent or great grandparent who suffered this infectious disease.Luckily, on the World TB Day of 2015, the occurrence of TB in Norway is relatively low (350-400 reported cases/year). We have antibiotics for treatment, and most of the Norwegian cases are actually non-active, non-contagious so-called latent TB.
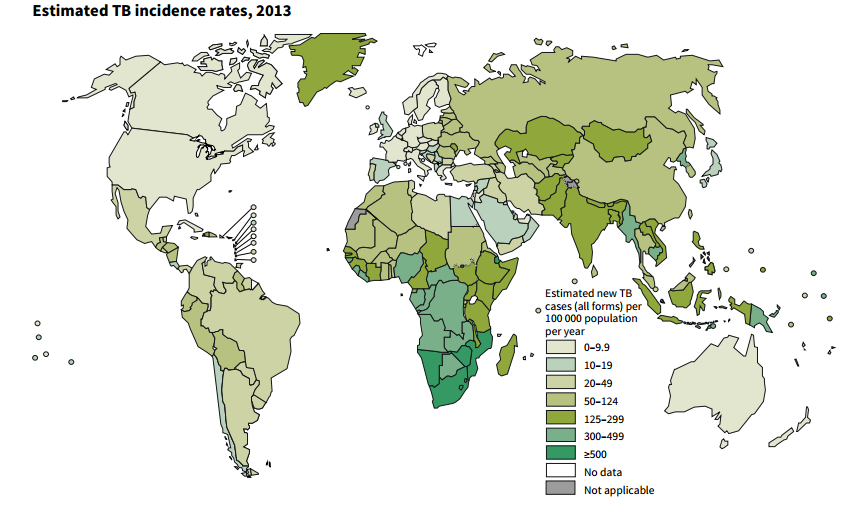
However, and here is why we need a World TB Day, globally TB is still a gigantic public health problem! In fact, only beaten by HIV/AIDS, TB is the deadliest infectious disease in the world. World Health Organization reports that 1.5 million people died from TB in 2013. That is almost every third Norwegian. The increase of antibiotic-resistant bacteria is at the same time a major emerging threat to human health, and TB resistant to our current drugs is on a rise. We urgently need new drugs for TB treatment.
To develop a new antibacterial drug is a time consuming process. It often starts with a large screen searching for compounds that kill the pathogen in question. Hit compounds are then typically optimized further, and for rational drug design purposes it is important to identify how the compound actually kills the bacteria. In our study, recently published in Antimicrobial Agents and Chemotherapy, we found the apparent mechanism of a new compound (PZP) that kills the TB-causing bacterium Mycobacterium tuberculosis. And the mechanism caught us by surprise.
A relatively new method used to identify the drug target and the mechanism of a new potential drug is to sequence the whole genome of bacteria that shows resistance to the compound in question. For instance, the mechanism of Bedaquiline, which is the first new TB drug on the marked in over 40 years (!), was discovered using this method. Genome sequences of M. tuberculosis resistant to Bedaquiline revealed mutations in the enzyme that provides the bacteria with energy; ATP synthase. This finding subsequently led to the discovery that Bedaquiline binds and inhibits the pathogen’s energy production unit.
Likewise, TB bacteria resistant to the new anti-TB compound we are interested in, PZP, were genome sequenced. The mutations discovered mapped to a gene that is important for the bacteria to take up iron from the surroundings. As for us humans, M. tuberculosis needs iron to live. Could it be that PZP binds and inhibits this iron uptake protein of M. tuberculosis so the bacterium cannot get a hold of the iron it needs? Just like Bedaquiline binds and inhibits ATP synthase and starves the bacterium for energy? We set out to confirm this hypothesis, however, step by step it became clear that our theory failed. PZP did not target iron uptake. Puzzled by this finding, the sharp chemists on our team did another discovery; PZP is in fact an iron chelator! That means, PZP can strongly bind to iron. So, instead of inhibiting bacterial uptake of iron, PZP seems to enter the bacterial cells and bind the iron the bacteria has already taken up, making it unavailable for the bacteria to use. PZP apparently starves the TB bacteria for iron from the inside!
Together with our collaborators at research institutions in Boston, Rome, Texas, Seattle and New York we learned an important lesson from this study, important also for other researchers in the drug development field. Things are not always as they seem. The gene that maps to resistance towards an antimicrobial compound is not necessarily the target of the compound. But, even if it is not the target, to identify such genes can give us crucial hints about the true mechanism of the new drug candidate. As for us; we were successfully pointed in the direction of iron metabolism.
Reference: A Novel Antimycobacterial Compound Acts as an Intracellular Iron Chelator, Antimicrobial Agents and Chemotherapy, April 2015 vol. 59 no. 4.