Blogger: Egil Lien, CEMIR/NTNU, UMass Medical School

You usually don’t think about the plague when you take a couple of extra hot dogs from the grill – which in turn may contribute to you putting on a few extra kilos – but the truth is that obesity, which can lead to type 2 diabetes, is also associated with inflammation.
Infectious diseases remain one of the leading causes of death in the world, and illnesses such as malaria and HIV take many lives each year. Developing countries are particularly overrepresented when it comes to places that are hit hard by infectious diseases.
But the situation today is nothing compared to what happened in Norway and the rest of Europe in the 1300s. The Black Death struck at full strength around 1347-1348, and in 1349 in Norway. When the pandemic (an epidemic that affects a large part of the globe) ended a few years later, it is estimated that 30-60% of the European population was gone. Several waves of plague epidemics followed in the years to come, until about 1654. In Norway, farms and hamlets were desolate and the country was left in a weakened state, which probably contributed to Norway’s forced union with Denmark.
The plague had a major effect on the social fabric of many European countries. The Black Death was caused by the bacterium called Yersinia pestis, which today still infects several thousand people worldwide, but is not currently found in Europe.
We can learn a lot by studying Yersinia pestis, one of the most dangerous bacteria we know. For example, at CEMIR we use Yersinia pestis as a model system to understand how this and other bacteria try to avoid detection by the immune system when they enter the body.
We can learn a lot by studying Yersinia pestis, one of the most dangerous bacteria we know. For example, at CEMIR we use Yersinia pestis as a model system to understand how this and other bacteria try to avoid detection by the immune system when they enter the body.
The plague bacterium has several tricks up its sleeve. It kills immune cells and modifies its surface so that the innate immune system responds weakly to the infection and doesn’t wipe out the bacterium. It also uses a “needle” to make small pores in the body’s immune cells and inject proteins into the cells to block immune responses and other cell functions. This means that bacteria can multiply more and less unrestrained in the body, and patients afflicted by plague may have especially large amounts of bacteria in their bodies.
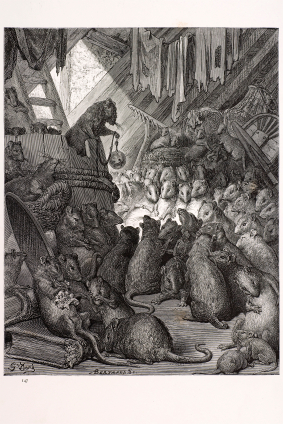
The rats have been blamed for spreading The Black Death http://en.wikipedia.org/wiki/Black_Death_in_England
We are working to figure out what specific immune responses are blocked and are underdeveloped during an infection such as this. We do this by trying to influence the system to provide an increased immune response, increasing inflammation, so that bacteria can still be killed by immune cells. This knowledge can be very important as we try to develop therapies and vaccines for a whole host of other infections.
We are working to figure out what specific immune responses are blocked and are underdeveloped during an infection such as this. We do this by trying to influence the system to provide an increased immune response, increasing inflammation, so that bacteria can still be killed by immune cells. This knowledge can be very important as we try to develop therapies and vaccines for a whole host of other infections.
But what on Earth could this have to do with obesity and diabetes? You usually don’t think about the plague when you take a couple of extra hot dogs from the grill – which in turn may contribute to you putting on a few extra kilos – but the truth is that obesity, which can lead to type 2 diabetes, is also associated with inflammation. The body is simply out of balance, and the extra fat tissue may contain immune cells that have been activated.
At CEMIR we have found that some of the same immune reactions that are initiated by an infection are also initiated when mice become obese. That means that inflammation, which is a helpful response of the body to an acute infection, can become chronic in association with excess weight. This can be harmful to the body and can contribute to the development of symptoms of type 2 diabetes, such as impaired glucose tolerance. We are trying to determine the reason behind this and will see if we can slow these symptoms by slowing the inflammation itself.
1. Allen, I.C. et al. NLRP12 suppresses colon inflammation and tumorigenesis through the negative regulation of noncanonical NF-kappaB signaling. Immunity 36, 742-754 (2012).
 The official opening of the Norwegian University of Science and Technology’s four new centres of excellence (CoE) will take place on Monday 10 June. CEMIR, the Centre of Molecular Inflammation Research, is one of these new centres. CEMIR researchers will study new mechanisms that set off inflammatory responses. We hope this will provide us with information that could help in the development of new treatment methods and the diagnosis of diseases in which inflammation plays a crucial role. You can read more about CEMIR at http://www.ntnu.edu/cemir
The official opening of the Norwegian University of Science and Technology’s four new centres of excellence (CoE) will take place on Monday 10 June. CEMIR, the Centre of Molecular Inflammation Research, is one of these new centres. CEMIR researchers will study new mechanisms that set off inflammatory responses. We hope this will provide us with information that could help in the development of new treatment methods and the diagnosis of diseases in which inflammation plays a crucial role. You can read more about CEMIR at http://www.ntnu.edu/cemir
In June there will be more blogs from CEMIR researchers.
