by Yucel Karabiyik, researcher at CIUS

Yucel Karabiyik
Physical examination at the doctor’s office often involves palpation where the physician tries to feel the location, size, shape and stiffness of masses or organs in the body by touching. Sometimes, even the patients themselves can notice lumps or abnormalities in their body and refer to a physician. Examples include palpation for masses or abnormalities in breast, spleen, liver and thyroid. However, this process has its limitations. It is subjective, meaning that the diagnosis is highly dependent on the skills of the physician and it is not sensitive to small and deep tumors. Therefore, nowadays it is usually used for preliminary screening before referring the patient for further investigation.
Elastography is an imaging modality that can overcome these limitations. It is a quantitative method (as opposed to palpation) and the estimated tissue stiffness can sometimes be directly related to certain diseases or even stages of a disease. For instance, it has been found that the stiffness of liver estimated with elastography can be used for staging of liver fibrosis.
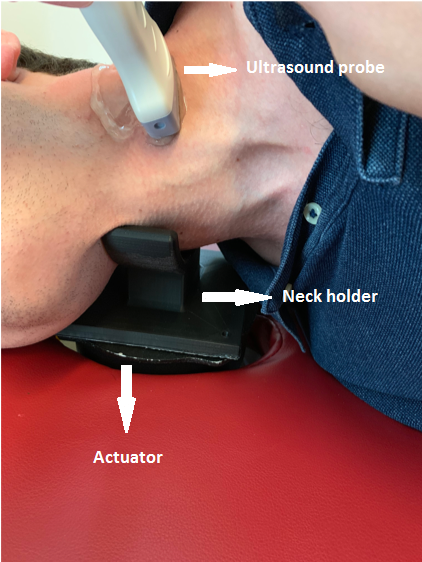
Figure 1
The method is based on generating very small amplitude displacements in the tissue and estimating how fast these displacements propagate in the form of waves. The stiffer the tissue, the faster the displacements propagate. The displacements are generated with actuators, which can be a loud speaker, an electrodynamic shaker or another kind depending on the application. The first step after creating the displacements is to image and estimate the displacement amplitudes. Diagnostic imaging techniques, magnetic resonance imaging (MRI) and medical ultrasound imaging are used for recording these displacements. Both techniques have their advantages and limitations. MRI can detect displacements in 3-D with good signal-to-noise ratio. However, it is costly and the scanning time is long compared to medical ultrasound. Ultrasound on the other hand, is portable, cheaper and faster but the displacement estimations have lower signal-to-noise ratio. Figure(1) shows an image from an ultrasound thyroid scanning. A 3-D printed neck holder is placed on the actuator and displacements are imaged using a linear ultrasound probe.
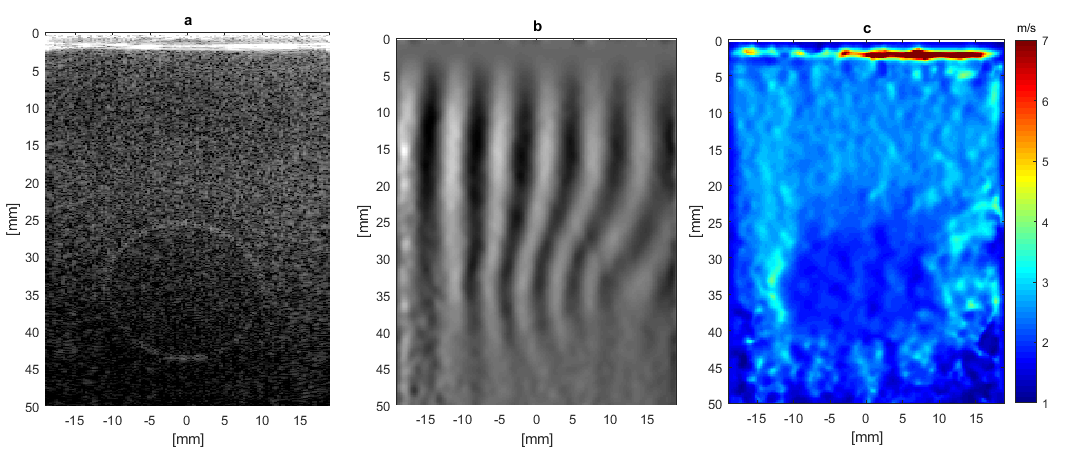
Figure 2
Figure (2) shows an example from a phantom recording. The shaker was driven with a 400 Hz sinusoidal signal. The phantom consists of inclusions with different stiffness values embedded in a tissue mimicking material. Figure (2).a shows an inclusion that is softer than the background material located between 25 – 45 mm depth. Wave images can be generated as shown in Figure (2).b after displacement estimation. One can see that in the upper part of the image, i.e., above 25 mm, the waves have constant wavelength. This wavelength is dependent on the stiffness of the material. Waves in the inclusion have shorter wavelengths which tells us that the material here is softer and the wave propagates with a lower velocity. Figure(2).c shows the final velocity estimations. As can be seen from the image, the part of the image where the inclusion is located has lower wave propagation velocity than the background. Using this velocity information, we can estimate the stiffness of the material.
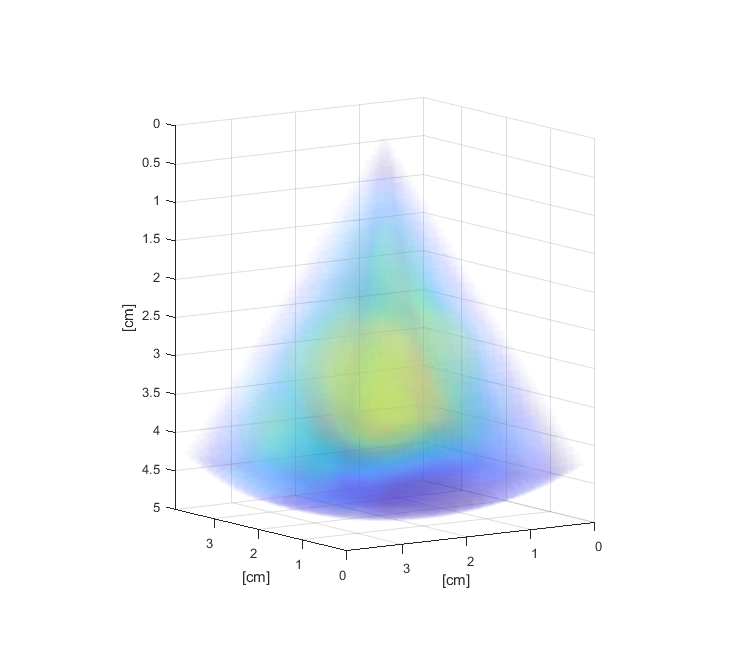
Figure 3
Figure (3) shows the result of a recording from a stiff inclusion in the phantom. A 3-D ultrasound probe used for the recording and the stiff inclusion could be reconstructed in 3-D. Our main goal is to apply this technique in cardiac imaging and estimate the stiffness of the myocardium in 3-D using ultrasound imaging. Estimation of myocardial stiffness may potentially help in understanding and diagnosing of relaxation and contraction abnormalities in the heart.
