Bloggers: Hanna Maja Tunset, PhD candidate, Eugene Kim, PostDoc,
MR Cancer group, Department of circulation and medical imaging
October is nearly over. The good news is that Christmas season is just around the corner. The bad news? This is the final post from the MR Cancer group in our blog series for breast cancer awareness month! If you missed the first two blogs, you can check them out here: A new cure for breast cancer? and Could breast cancer metabolism reveal new therapeutic targets?
Breast cancer is not just one disease, and different breast cancers need different treatment. Targeted treatment according to the type of tumor has increased breast cancer survival for a lot of patients. However, around 15 % of breast cancer patient have what we call triple negative breast cancer (TNBC), which does not respond to currently available targeted therapies. This subtype also tends to be highly aggressive, develop at a younger age, and have poorer prognosis compared to other types. Going against the overall trend in breast cancer, survival rates for TNBC have not increased in the past few decades. So, new targeted therapies for TNBC are in high demand.
One way of finding a good therapeutic target is to look for something that is unique to that particular disease. We have previously identified that the inflammatory enzyme cytosolic phospholipase A2, or cPLA2, is overly active in TNBC as compared to other breast cancers. We wanted to see if inhibiting cPLA2 could be an effective treatment. So we teamed up with Berit Johansen, a professor at the NTNU Department of Biology and CSO of Avexxin AS, a Trondheim-based start-up company developing a line of cPLA2 inhibitors intended to treat inflammatory diseases like psoriasis and rheumatoid arthritis.
We tested one of their drugs, AVX235, in a mouse model of TNBC, and the results look promising. Tumors in mice treated with the drug only reached 1/3rd of the size of untreated control tumors after 19 days of treatment.
But how does AVX235, an anti-inflammatory drug, inhibit tumor growth?
Targeting the link between inflammation, blood vessels, and cancer
Cytosolic phospholipase A2 is highly involved in both acute and chronic inflammation in the body. In 1863, Rudolf Virchow, the father of cellular pathology, theorized that cancer was caused by chronic inflammation. Over the years, research has revealed close links between inflammation and cancer. American pathologist Harold Dvorak went as far as to describe tumors as “wounds that do not heal”. A major component of inflammation and wound healing is angiogenesis – the growth of new blood vessels. Angiogenesis is a hallmark of cancer and is observed in most solid tumors. As a tumor grows, it produces blood vessels that deliver the oxygen and nutrients necessary to sustain it.
Our study suggests that cPLA2 plays an important role in angiogenesis in TNBC. We found that AVX235 reduced the amount and size of blood vessels in the tumors. High-resolution CT images showed that large portions of tumors treated with AVX235 did not have a blood supply.
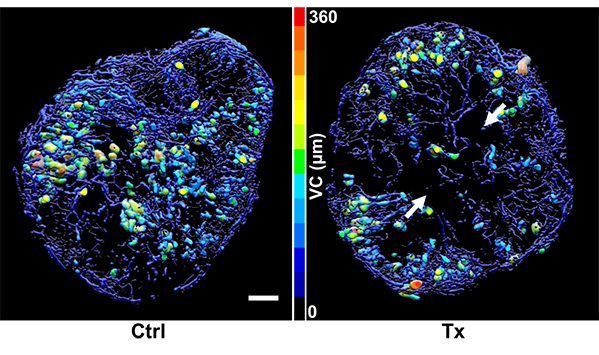
CT-based images of representative tumors from control (Ctrl) and treated (Tx) groups, color-coded for vessel caliber (VC), i.e. vessel diameter – the more yellow or red, the larger the vessel. Note the lack of vessels in large areas of the treated tumor (arrows).
We also examined tumor tissue under the microscope, after staining for certain factors that could reveal if blood vessel cells were dividing. Treated tumors had fewer actively growing blood vessels. This indicates that blocking cPLA2 activity hindered the cancer’s ability to produce new blood vessels, resulting in tumors that were under-fed and unable to grow as they normally would.
Next steps towards improving treatment of TNBC
We are still in the early phases, but our initial results show that inhibition of cPLA2 may be a strategy for targeted therapy of TNBC. Continuing our collaboration with Avexxin, we are currently trying to find out more about how this may work. By using breast cancer cells grown in a flask as a model system, we can detect responses on a cellular level, like alterations of metabolism, how fast the cells grow, and their ability to invade new tissues.
Over the past decade, there has been an increasing interest in cPLA2 as an important player in the progression of various cancers, including breast cancer. We hope our research in this field will contribute towards providing a much-needed targeted therapy for triple negative breast cancer patients.
The results from this study was published in BMC Cancer.
This work was funded by the liaison committee between the Central Norway Regional Health Authority and the Norwegian University of Science and Technology (NTNU), the Norwegian Cancer Society, the Research Council of Norway, and Avexxin AS.

From the back (left to righ): Astrid Jullumstrø Feuerherm, Siver Moestue, Jana Kim, Eugene Kim, Berit Johansen and Hanna Maja Tunset

