Blogger: Jana Cebulla
PhD Candidate at MR Cancer group
Angiogenesis is the formation of new blood vessels from pre-existing vessels. This process takes place during wound healing, but is also essential during the development of certain diseases, such as cancer.
In order to grow beyond a size of 1-2mm, tumors send out chemical signals telling nearby blood vessels to send new vessels in the direction of the tumor. This way, the cancer cells can get sufficient supplies of oxygen and nutrients. Angiogenesis has also been found to help cancer spread to other parts of the body (i.e. metastasize).
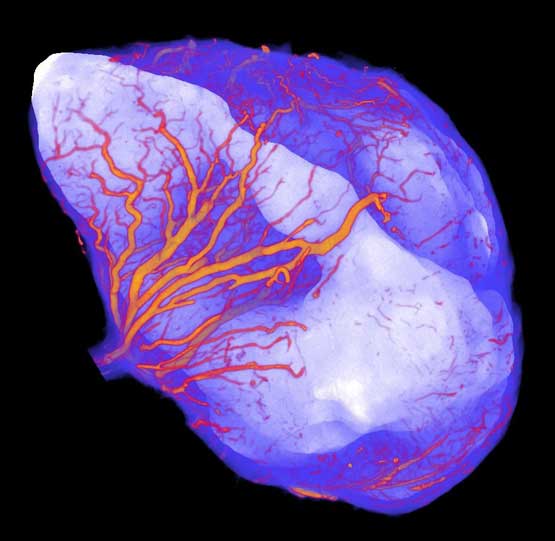
Blood vessels (orange) that are recruited by a tumor (white) which was grown on the leg of a mouse (surrounding “healthy” tissue in blue). Photo: Jana Cebulla
Hopefully, in the future the worldwide research on angiogenesis can help put together all the pieces in the puzzle and describe how angiogenesis in cancer is regulated and how we can influence it with drugs in order to treat cancer patients more effectively.
Since angiogenesis plays such a crucial part in cancer development, a large number of drugs have been developed that directly or indirectly target the tumor vasculature.
In theory, drugs blocking angiogenesis should be magic bullets, killing the tumors while causing relatively little adverse effects. In practice, they have turned out to be less effective than expected.
Clinical experience indicates that anti-angiogenic drugs increase survival only in some cancer types, and only in a limited number of patients. In order to identify these patients, we need a better understanding of how these drugs work. More research is needed to put together all the small details in the complicated pathways that these drugs affect. In addition to this, we need to increase our knowledge about how the vasculature itself reacts to those drugs. We can get some clues from studying cells in flasks, but solid tumors are complex “organs” with a characteristic local microenvironment. Specialized non-invasive medical imaging methods are therefore increasingly used to visualize changes in tumor vascularization over time or during treatment.
Angiogenesis research around the world
Several labs at NTNU and many labs around the world are focusing their research on angiogenesis. One of the main research areas of the MR Cancer group at NTNU, headed by Tone F. Bathen is to image angiogenesis using Magnetic Resonance Imaging (MRI) which can be used both in preclinical studies with animals and in clinical studies with patients to investigate tumor blood vessels.
For over three years I have now been a part of the MR Cancer group as a PhD student where I have the opportunity to work on exciting projects. My first introduction to the field of angiogenesis, however, was during a research stay as a Master Student at The Johns Hopkins University School of Medicine in Baltimore, USA in Dr. Arvind Pathak’s imaging lab. Dr. Pathak was the first to use high-resolution micro-MRI to image tumor blood vessels and his lab has pioneered the development of multimodality and multiscale angiogenesis imaging in cancer.
Fascinating images
At Johns Hopkins, I used several independent imaging modalities that were combined to gain a composite picture of the blood vessels in a breast cancer model at different spatial scales. At the macroscopic scale we used in vivo MRI, which is also applicable in patients. Although the resolution of in vivo MRI is not good enough to resolve small blood vessels in the tumor, with certain imaging techniques we are able to produce “maps” of the tumor blood volume or the average vessel size. In addition, MRI allows us to indirectly look at the cellular properties of the tumor such as cell density.
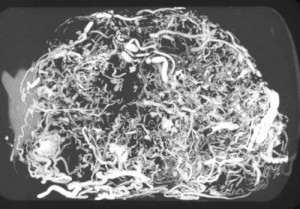
At the microscopic scale, we used micro-computed tomography (CT) to directly visualize the blood vessels of the whole tumor at 8 µm resolution (which is approximately the diameter of a red blood cell). Due to the different resolutions and information that in vivo MRI and micro-CT yield, we then used ex vivo micro-MRI in addition, which allowed us to co-register the data and combine the information.
This procedure not only resulted in spectacular images but enabled us to visualize and characterize the chaotic vascular network of the tumor, with a lot of twisting, turning and immature vessels in the outer regions and relatively few vessels in the center. We were also able to demonstrate how a central area of dying tumor cells (i.e. necrosis) was far away from the nearest perfused blood vessels. This again emphasizes the importance of angiogenesis for the development of cancer.
This exciting work was published in the journal Angiogenesis and our images were featured on the cover of the journal.
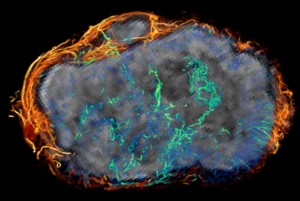
Ovarian tumor grown on the leg of the mouse in grey (MRI) overlaid with blood vessels from micro-CT images that are densely surrounding the tumor (orange) and feeding into it to form a chaotic network (green/blue). Photo: Jana Cebulla
The MR Cancer group at NTNU is collaborating with Dr. Pathak’s lab, and in a recent project we were able to use the developed methods to look at tumor angiogenesis in ovarian cancer models. We are also trying to quantify changes in tumor blood vessels that happen during cancer treatment. We hope that our research will shed more light on how tumor blood vessels react to those treatments and how we can fight cancer using novel drugs.
Hopefully, in the future the worldwide research on angiogenesis can help put together all the pieces in the puzzle and describe how angiogenesis in cancer is regulated and how we can influence it with drugs in order to treat cancer patients more effectively.
___
The research stays at The Johns Hopkins University School of Medicine were supported by an Otto Bayer Scholarship from the Bayer Foundation, a Leiv Eiriksson mobility grant from the Research Council of Norway and a MedIm Research and Travel Grant.