Blogger: Morteza Esmaeili
Postdoctoral Fellow at MR Cancer Group, NTNU
A new non-invasive method can identify a special mutation in a type of brain tumor called gliomas. This unique test can assist in research towards new treatments that target cancer cells in glioma patients carrying this mutation. The new method is developed by my colleagues and me at MR Cancer Group at NTNU and researchers at the Departments of Radiology and Pathology of Radboud University Medical Center in Nijmegen. We believe it is an important step towards improved tools for the diagnosis and treatment evaluation of brain tumor patients.
Gliomas are common subtypes of primary brain tumors that originate from glial cells in the brain. There are different grades of gliomas, indicating their degree of aggressiveness; however, they are most often classified as “low-grade” or “high-grade” gliomas. Glioblastomas are the most aggressive type of gliomas. Various types of gliomas have been identified, and they have different clinical behavior and response to treatment. This means there is an urgent need for more accurate and precise diagnosis, prognosis, and therapy monitoring tools.

Gliomas are common subtypes of primary brain tumors that originate from glial cells in the brain. A new non-invasive method can identify a special mutation in gliomas. (Photo: Geir Mogen/NTNU)
Conventional anatomical imaging methods, such as magnetic resonance imaging (MRI) (Figure 1), provide limited information on tumor characterization and prognosis. Advances in personalized patient management and new drug treatments for brain tumors have generated increasing demand for reproducible, non-invasive, quantitative imaging biomarkers.
Recent developments have concentrated on the role of physiological and metabolic MRI, such as magnetic resonance spectroscopy (MRS, see an example in Figure 2), and other molecular imaging methods in understanding the metabolic processes associated with tumor growth and progression. These studies have indicated that cancer cell metabolism, contrary to the metabolism in normal cells, is modulated and reprogrammed to facilitate additional/excessive demands for biomass generation and rapid cellular growth and proliferation. This particular characteristic of cancer cells can be targeted as a “weak point” to kill these cells.
This particular characteristic of cancer cells can be targeted as a “weak point” to kill these cells.
Furthermore, the utility of various techniques in distinguishing between aggressive and benign tumors, tumor grading, and treatment response evaluation and monitoring are also of interest.

Figure 1: Conventional MR imaging of glioblastoma. Tumor regions can be identified by different MR contrasts; For example, (A) T1-weighted pre-contrast exhibit a low-intensity lesion in the left frontal lobe region (yellow arrow), (B) post-contrast MR image demonstrates a focus of enhancement in that area, (C) and T2-weighted MR image shows increased-intensity at the same region. These MR techniques enable non-invasive imaging and diagnosis of tumor lesions in the brain. Illustration is adapted from Ahmed R. et al. Cancer Manag Res, 2014 (with permission).
During our study, we uncovered a new imaging biomarker to identify glioma subtypes with different prognosis and therefore this biomarker may be used for a better clinical management, avoiding extra cost for patients and communities. More specifically the biomarker concerns metabolite levels associated with a mutated IDH gene found in more than 70% of the brain tumors classified as low-grade gliomas and secondary gliomas. Glioma patients with this mutation actually have a better prognosis.
In particular, with our MRS technique we observe the indirect effect of the mutation in the IDH1 gene on the level of some phospholipid metabolites, which can be considered a molecular “finger print” for this mutation. These metabolites are major components of phospholipid metabolism in the synthesis of cancer cell membranes.
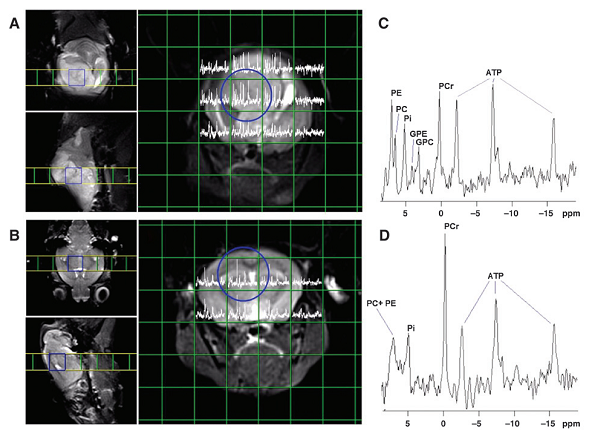
Figure 2: MR spectroscopy provides information additional to conventional MRI. T2-weighted MR images of a mouse brain with glioma tumor (top, A) and a healthy mouse brain (bottom, B), and corresponding MRS data from area of interest (blue circles, C and D). MRS detects signals for different metabolites in normal brain and tumor tissue. In particular phospholipid metabolites are of interest to characterize brain tumors. (from left to right); PE, phosphoethanolamine; PC, phosphocholine; GPE, glycerophosphoethanolamine; GPC, glycerophosphocholine. Adapted from Esmaeili M. et al. Cancer Res. 2014 (with permission).
To be a bit technical: IDH1 acts in an energy-generating pathway known as the citric-acid cycle, and the IDH1 mutations associated with cancer causes a metabolite called 2-hydroxyglutarate to accumulate. IDH1 catalyzes the conversion of isocitrate into α-ketoglutarate, a reaction that takes place in energy-generating metabolic pathways. Most remarkable is that the mutated IDH1 enzyme has acquired the capacity to produce 2-hydroxyglutarate, which can accumulate in high concentrations in gliomas with the mutation. 2-hydroxyglutarate is commonly called an oncometabolite. Our finding shows that the mutation also alters lipogenesis in brain cancer cells. Phospholipid metabolism is a major network supporting cellular lipogenesis and cell membrane turnover.
The discovery of the IDH1 mutation has generated such intense interest that pharmaceutical companies are keen to find drugs that target mutant IDH1 gliomas
The discovery of the IDH1 mutation has generated such intense interest that pharmaceutical companies are keen to find drugs that target mutant IDH1 gliomas, with some companies focusing exclusively on targeting cancer metabolism. The findings of this study and those published recently on IDH related metabolism could be used in the development of drugs for cancers with these mutations. In addition, these findings enable the detection through non-invasive imaging of the direct metabolic consequence of a genetic mutation in a cancer cell. This offers a potential new tool in the management of brain tumor patients.

