By Marlene Iversen Halvorsrød, PhD Candidate at CIUS
Treatment of ischemic heart disease has improved considerably the last decades. Not only the treatment itself, but also timing of treatment has been of great importance for this success. Nevertheless, ischemic heart disease is still the leading cause of death in the world.
 The heart muscle, as every other muscle in the body, needs oxygen to maintain proper function. The coronary arteries supply the heart muscle with oxygenated blood. Ischemic heart disease is caused by stenosis or totally occlusion of this arteries and thereby reduced amount of available oxygen. This lack of oxygen can lead to permanent heart muscle damage. The longer the muscle have no available oxygen, the worse the damage will be. Treatment of ischemic heart disease is based on opening stenotic or occluded arteries to improve the accessibility of oxygen. Either by invasive blocking or medical (fibrinolytic) treatment. Time from debut of symptoms to treatment is a crucial determinant for success. The shorter ischemic time, the less heart muscle damage. After 6 hours without oxygen, the majority of heart muscle cells are likely to suffer from irreversible damage.
The heart muscle, as every other muscle in the body, needs oxygen to maintain proper function. The coronary arteries supply the heart muscle with oxygenated blood. Ischemic heart disease is caused by stenosis or totally occlusion of this arteries and thereby reduced amount of available oxygen. This lack of oxygen can lead to permanent heart muscle damage. The longer the muscle have no available oxygen, the worse the damage will be. Treatment of ischemic heart disease is based on opening stenotic or occluded arteries to improve the accessibility of oxygen. Either by invasive blocking or medical (fibrinolytic) treatment. Time from debut of symptoms to treatment is a crucial determinant for success. The shorter ischemic time, the less heart muscle damage. After 6 hours without oxygen, the majority of heart muscle cells are likely to suffer from irreversible damage.
Classical symptoms of ischemic heart disease as heart attack are chest pain with radiation to neck and shoulder, shortness of breath and sweating. The symptoms are often related to physical activity. But this stenotic or occluded artery manifest with a great variability of symptoms that makes the diagnostic process hard and sometimes time consuming.
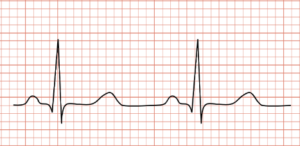
In addition to a patient’s symptoms, the most important quick diagnostic tool is the electrocardiogram (ECG). ECG was first used in late 1800 and is still a cornerstone in diagnosing ischemic heart diseases. ECG records the electrical signals through the heart. We classify heart attacks by the look of the ECG. A patient with chest pain and a certain pattern in ECG called ST-elevation, usually has an occluded artery and will be treated immediately. In some cases, patients lack this typical pattern in ECG, but have the same occluded artery. This group of patients does not have the same algorithm for immediate treatment and the treatment can be delayed. The consequence is more damaged heart muscles than necessary.
 A lot of effort is put down to solve this diagnostic puzzle. In our research group at CIUS (Centre of Innovative Ultrasound Solutions), NTNU (Norwegian University of Science and Technology) we try to take advantage of new advanced ultrasound technology to come closer to a solution. Ultrasound is routinely used in diagnosing ischemic heart disease today by looking at regional differences in how the heart muscle contract. To see this regional impairment, you need a trained eye and good image quality. This method is also highly subjective. We want to improve this diagnostic step by using new technology developed at NTNU with high frame rate imaging that gives better time resolution, tissue doppler that can measure the speed of the heart muscle in different regions, and 3D ultrasound.
A lot of effort is put down to solve this diagnostic puzzle. In our research group at CIUS (Centre of Innovative Ultrasound Solutions), NTNU (Norwegian University of Science and Technology) we try to take advantage of new advanced ultrasound technology to come closer to a solution. Ultrasound is routinely used in diagnosing ischemic heart disease today by looking at regional differences in how the heart muscle contract. To see this regional impairment, you need a trained eye and good image quality. This method is also highly subjective. We want to improve this diagnostic step by using new technology developed at NTNU with high frame rate imaging that gives better time resolution, tissue doppler that can measure the speed of the heart muscle in different regions, and 3D ultrasound.
We know that it is crucial that patients with blocked coronary artery get treatment immediately. We want to improve the way we select these patients. Medical technical solutions can take time to develop, but in time we hope to brake some barriers in this important issue concerning the world’s deadliest disease.