Bloggers: Anne Line Stensjøen, PhD Candidate, Department of Neuromedicine and Movement Science (INB), and Asta Håberg, Professor and Centre Director, Centre of Innovative Ultrasound Solutions (CIUS)
Glioblastomas are tumours that originate from brain tissue. It is both the most common and most aggressive type of brain tumour. The median survival at group level is only 10 months for glioblastoma patients in Norway, but it is difficult to predict how long an individual long patient will survive.
How fast brain tumours grow is important to know to make the best decisions with regard to treatment. Tumour growth can also tell us something about how aggressive the tumour is, and perhaps be used as a marker of prognosis. It has been difficult to assess tumour growth because it requires at least two magnetic resonance images (MRIs) of the brain before treatment is started.
 Anne Line Stensjøen has in her recent PhD at NTNU, performed the first large study measuring brain tumour growth, showing that glioblastomas grow rapidly when they are small and then more slowly as they get bigger. The growth rate was very fast with about 1.4% per day, which is equivalent to a doubling of the tumour size every 50 days across all the 106 glioblastomas investigated. This demonstrates the need for swift treatment of glioblastomas to prevent unnecessary growth.
Anne Line Stensjøen has in her recent PhD at NTNU, performed the first large study measuring brain tumour growth, showing that glioblastomas grow rapidly when they are small and then more slowly as they get bigger. The growth rate was very fast with about 1.4% per day, which is equivalent to a doubling of the tumour size every 50 days across all the 106 glioblastomas investigated. This demonstrates the need for swift treatment of glioblastomas to prevent unnecessary growth.
Importantly, tumour growth is associated with survival. Patients with slower growing tumours had a 4.4 higher chance of surviving for more than two years compared to patients with faster growing tumours. Measuring glioblastoma growth using MRI could therefore help estimating the prognosis for each patient.
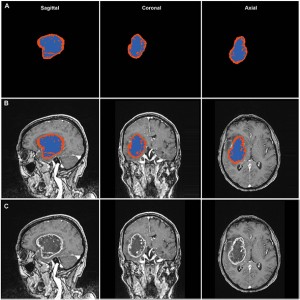
Stensjøen had to perform all tumour segmentations manually to find the tumour size. Manual segmentation is very labour intensive. Developing automated methods, for instance based on machine learning will make it possible to obtain growth measure in a more efficient manner suitable for clinical practice.
This work will be continued at the Centre for Innovative Ultrasound Solutions (CIUS) in the work package “Multimodal imaging and intervention” (WP5).

